Wishing you a safe and happy 4th of July from all of us at Arizona Clinical Trials, Arizona Liver Health, and VEN Centers as we celebrate the spirit of freedom and independence.

Honoring Our Heroes This Memorial Day.
Today, we pause to remember and honor the brave men and women who made the ultimate sacrifice in service to our country. Their courage, dedication, and selflessness will never be forgotten.
From all of us at Arizona Liver Health, Arizona Clinical Trials, and VEN Centers — we extend our deepest gratitude and respect to the heroes who gave everything for our freedom.
Today, on International Clinical Trials Day, our team proudly suited up in solidarity to recognize the global impact of clinical research. Clinical trials are at the heart of medical progress — helping bring new treatments to patients, especially those with limited access to care. From researchers and coordinators to every volunteer who chooses to participate, your efforts are driving healthcare forward and offering real hope to communities everywhere.
Stay informed. Stay involved. Make a difference.
Follow us to stay connected to the latest research opportunities and be part of the future of medicine.
#ClinicalTrialsDay #AdvancingCare #ACT #ALH #ResearchMatters #FutureOfHealth

Today on Clinical Trials Day, we’re celebrating the incredible impact of clinical research professionals like you. Your dedication is what drives medical progress forward — from the earliest stages of discovery to tomorrow’s breakthrough treatments. Every protocol you design, every data point you gather, and every patient you support brings us closer to improving health outcomes for individuals today and for generations to come.
Thank you for all that you do.
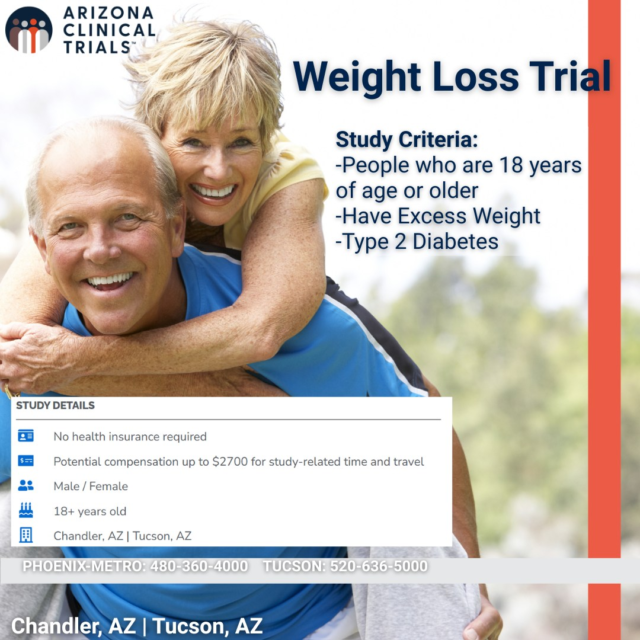
Obesity isn’t just about weight—it’s a complex health condition shaped by genetics, environment, and behavior.
At Arizona Clinical Trials, we’re conducting research studies in Phoenix, Tucson, and Flagstaff to help find better, more effective solutions. A BMI of 30 or higher is typically used to define obesity—but the real concern lies beneath the surface: how that extra weight affects the body’s organs, hormones, and overall health.
Why join a weight loss clinical trial?
-Early access to innovative treatments
-Ongoing health monitoring
-No insurance required
-May receive up to $2700 compensation for trial-related time & travel
-Help advance medical research
-Empower yourself with knowledge
If you’re 18 or older, have excess weight or type 2 diabetes, and are ready to take control of your health—this opportunity could be for you.
Visit azclinicaltrials.com to learn more and see if you qualify.
#ObesityAwareness #ClinicalTrials #ArizonaClinicalTrials #T2D #HeartHealth #ResearchForChange #ACTNow

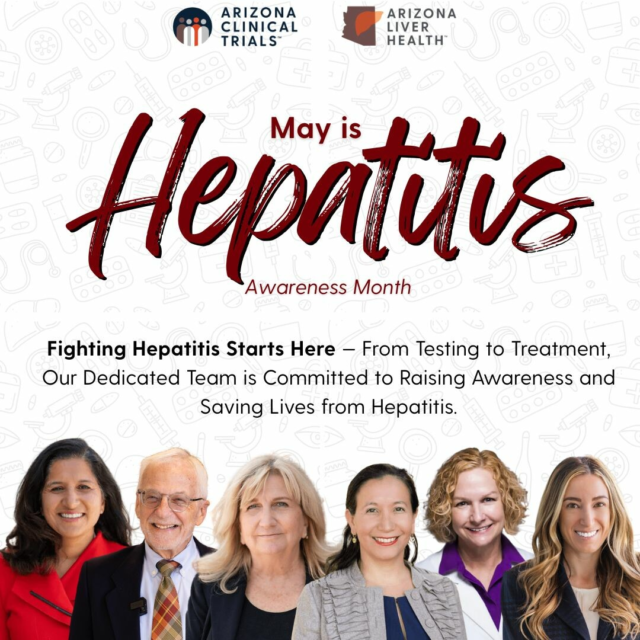
May is Hepatitis Awareness Month! At Arizona Clinical Trials and Arizona Liver Health we believe awareness leads to action—and action saves lives.
This month, we’re shining a light on hepatitis, and the importance of early testing, prevention, and access to care. Our dedicated team is here to walk alongside every patient—from screening to treatment—because fighting hepatitis starts with us.
Together, we’re building a healthier Arizona.
#HepatitisAwareness #LiverHealth #GetTestedAZ #ArizonaLiverHealth #ArizonaClinicalTrials
Today—and every day—we celebrate the incredible nurses who bring skill, compassion, and strength to every patient interaction.
At Arizona Liver Health, Arizona Clinical Trials, and VEN Centers, we’re proud to work alongside some of the most dedicated and inspiring nurses in healthcare. Your heart, hustle, and healing hands truly change lives.
Thank you for the care you give, the hope you inspire, and the impact you make. You are the backbone of our clinics—and real-life healthcare heroes.
A special shoutout to our amazing team:
@Karen Arendt, @Dylan Moore, @Tyler Padilla, @Racine Romero, @Ann Moore, Angie Coste, @Nicole Chrisman, @Marsha McCary, Vicki McIntyre, @Julia Melvin, Marianne Rosati, and Leslie Wojtowicz — your compassion and commitment never go unnoticed.
#NationalNursesWeek #ThankYouNurses #HealthcareHeroes #NursesWeek2025 #ArizonaLiverHealth #ArizonaClinicalTrials #VENCenters

Interested in participating in a clinical trial for weight management? This could be the opportunity you`ve been waiting for.
At Arizona Clinical Trials, we’re enrolling adults in a research study for chronic weight management using an investigational medication. If you’ve been struggling with excess weight or have type 2 diabetes, this could be the opportunity you`ve been waiting for!
-No health insurance needed
-You could earn up to $2,700 for trial-related time and travel
-You’ll get expert care from a dedicated medical team
-Locations in Chandler, Peoria, Tucson, and Flagstaff
We’re looking for individuals 18 and older—men and women—who are ready to take control of their health and be part of something that could help others too!
Ready to take the first step?
👉 Tap the link in bio to see if you qualify and sign up today!
#WeightLossJourney #ArizonaClinicalTrials #HealthyYou #TucsonAZ #ChandlerAZ #ClinicalTrialOpportunity #FeelGoodLookGood #StudyAndEarn
Ever wonder how new medicines get tested before they’re in your pharmacy? It all starts with clinical trials—and Arizona Clinical Trials is proud to be a part of the process!
Let’s break it down:
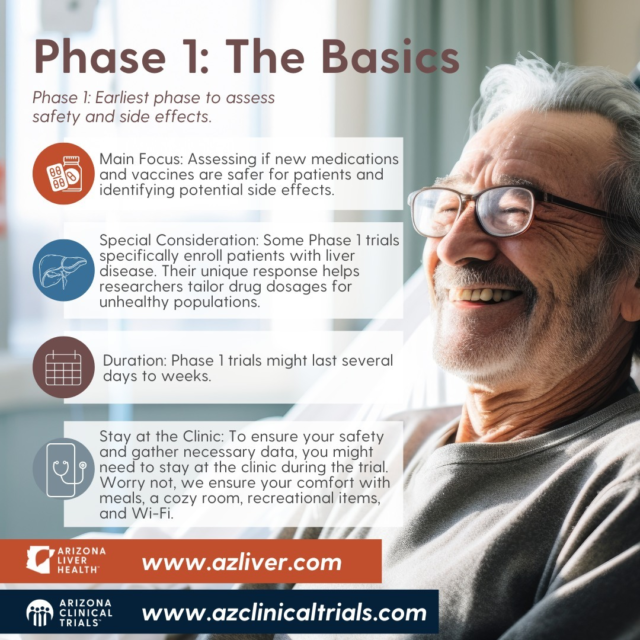
Phase 1 Trials – These are the first step. We test a new medicine with a small group of people to see if it’s safe and how the body handles it.
Phase 2 Trials – Now we’re checking if the medicine works for a certain condition and learning more about side effects. These studies involve more people than Phase 1.
Why join a trial?
✅ You may get access to new treatments before they’re widely available.
✅ You’ll be closely cared for by expert doctors and research teams.
✅ You’re helping move science forward—and that helps everyone!
We’re doing this important research right here in Arizona. If you or someone you know is curious about participating, we’re happy to answer questions. No pressure, just information!
Let’s build the future of medicine—together.
#ArizonaClinicalTrials #Phase1Trials #Phase2Trials #ResearchMatters #ClinicalTrials #AZResearch #HealthcareHeroes

In honor of World Liver Day 2025 on April 19, Arizona Liver Health, VEN Centers, and Arizona Clinical Trials are proud to join the global movement to raise awareness about liver health. This year’s theme, “Food is Medicine,” emphasizes the critical role of nutrition in maintaining liver function and preventing liver diseases.
A balanced diet rich in whole foods—fruits, vegetables, whole grains, and lean proteins—can significantly reduce the risk of liver conditions such as metabolic dysfunction-associated steatotic liver disease (MASLD). However, we acknowledge that access to nutritious food is not always equitable. It’s essential to advocate for policies and community initiatives that make healthy eating more accessible to all.
Join us in spreading the message that every meal is an opportunity to support your liver health. Together, we can make informed choices and advocate for a healthier future.
#WorldLiverDay #FoodIsMedicine #LiverHealth #ArizonaLiverHealth #VENCenters #ArizonaClinicalTrials
Today is World Health Day — A Global Call to Prioritize Prevention, Equity, and Awareness. At Arizona Liver Health (ALH), Arizona Clinical Trials (ACT), and VEN Centers, we stand united in our commitment to advancing global health through early detection, research innovation, and community-based outreach.
As awareness grows around chronic diseases, mental health, and the power of prevention, we’re proud to be part of a movement that brings healthcare closer to home—and to everyone.
On this World Health Day, take a moment to invest in your health.
✔️ Get screened.
✔️ Join a study.
✔️ Protect your future.
Because when we care for ourselves and each other, we move one step closer to a healthier, more equitable world.
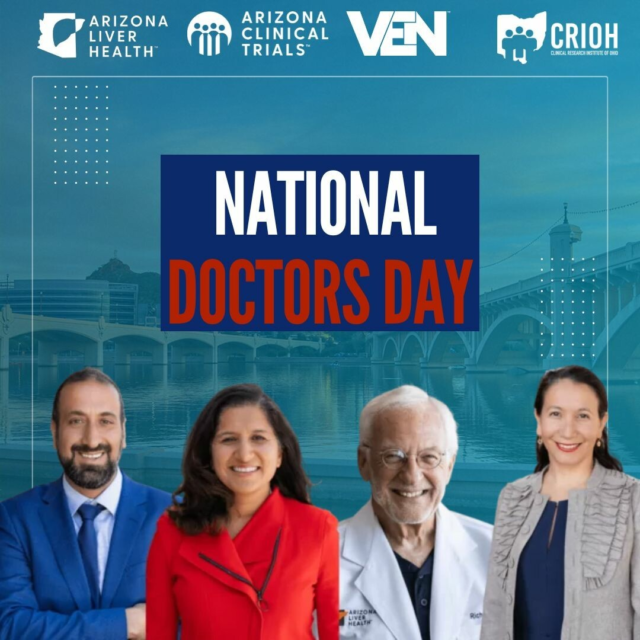
Yesterday was National Doctors’ Day, and we couldn`t let it pass without celebrating the incredible physicians who make a difference every single day.
A heartfelt thank you to Dr. Anita Kohli, Dr. Naim Alkhouri, Dr. Richard Manch, Dr. Yessica Sachdeva, and Dr. Aimee Bachelier—your expertise, compassion, and unwavering commitment to patient care inspire us all.
Fun Fact: National Doctors’ Day has been celebrated on March 30 since 1933, chosen to honor the first use of ether anesthesia in 1842—one of many innovations that continue to shape modern medicine.
To all doctors: we see you, we appreciate you, and we thank you!
#NationalDoctorsDay #ThankYouDoctors #HealthcareHeroes #TeamALH #ArizonaClinicalTrials #ArizonaLiverHealth #VENCenters
This week marks the beginning of Black History Month, a month-long event to celebrate the history, culture, and contributions of African Americans to our nation. Acknowledging the profound impact and indelible legacy of Black history, because understanding the past is key to building a more inclusive future.
#BlackHistoryMonth #ALH #ACT #VEN #CRIOH
Today, we honor the legacy of Dr. Martin Luther King Jr., a leader whose courage, vision, and unwavering commitment to justice and equality continue to inspire us. Let us reflect on his powerful message of unity and work together to build a brighter, more equitable future for all.
#mlk #Ihaveadream #equality
This holiday season, we’re filled with gratitude for our incredible community and the opportunity to make a positive impact together. May your holidays be bright, your hearts full, and your moments with loved ones unforgettable.

Happy Thanksgiving! We’re grateful for our amazing team, patients, and partners who make everything we do possible. Wishing you and your loved ones a joyful and peaceful holiday!

Arizona Clinical Trials is excited to announce the opening of our new state-of-the-art clinic in Tucson, bringing innovative health solutions closer to you! We’re looking for community members aged 65 and over in the greater Tucson area to participate in an important Norovirus clinical trial. Your involvement can help shape the future of healthcare and protect our communities.
Why join?
-Make a real impact on public health
-Be part of a professional and compassionate team
-Access cutting-edge healthcare insights
Help us advance Norovirus research by joining this exciting trial! To learn more or see if you qualify, visit: https://azclinicaltrials.com/norovirus-trial/
#ArizonaClinicalTrials #TucsonAZ #Norovirus #ClinicalTrial

Today, we honor those who served with courage and commitment. Thank you to all veterans for the sacrifices you`ve made to protect our freedom. #VeteransDay #ThankYouVeterans

Happy Halloween from Arizona Clinical Trials! 🎃 Don’t let your health give you a fright—participate in research today for a fang-tastic future. Have a safe and spooktacular Halloween

Join me as I chat with some of our amazing research team members to find out why clinical trial participation is so vital.
.
.
.
Interested in joining a clinical trial? Click the link in our bio to see our currently enrolling studies!
#act #clinicaltrials #advancingmedicine #makingadifference

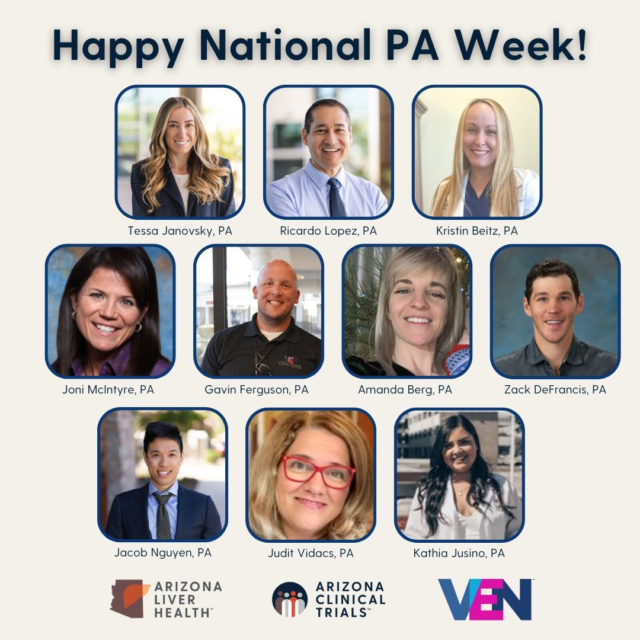
Happy National PA Week!
This week, we`re celebrating our wonderful Physician Assistants, who play a key role in your care. Their dedication, compassion, and expertise help make sure you receive the best possible treatment every day.
From listening to your concerns to working alongside our team, they are truly advocates for your health. We are grateful for their hard work and the difference they make in the lives of our patients.
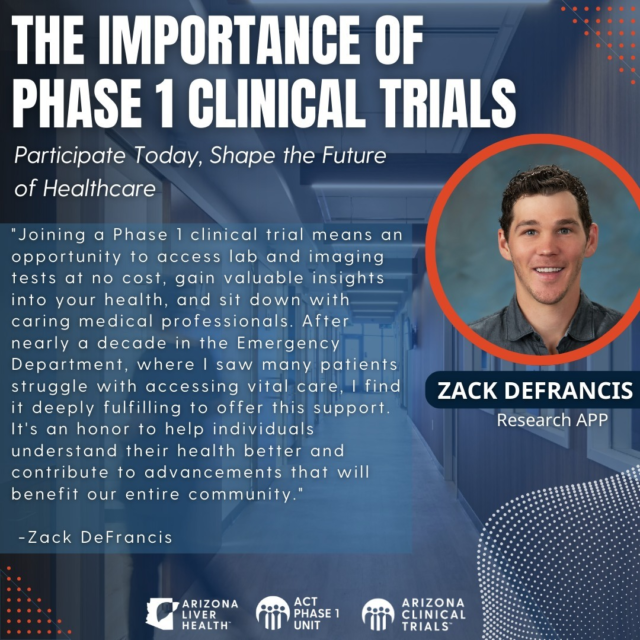
Participating in a Phase 1 clinical trial is a chance to make a real difference. By joining a trial, you gain valuable insights into your health through lab and imaging tests at no cost, while contributing to the development of breakthrough treatments that will benefit your entire community.
As Zack DeFrancis, Research APP at Arizona Clinical Trials, explains:
"After nearly a decade in the Emergency Department, where I saw many patients struggle with accessing vital care, I find it deeply fulfilling to offer this support. It`s an honor to help individuals understand their health better and contribute to advancements that will benefit our entire community."
Your participation in a Phase 1 trial not only empowers you with knowledge about your own health, but it also plays a critical role in driving medical progress forward. Your involvement today helps shape the future of healthcare for everyone.
For more information, contact us at https://azclinicaltrials.com/phase-1-trials/
#ClinicalTrials #HealthcareInnovation #MedicalResearch #CommunityHealth #Phase1 #FutureOfMedicine #ArizonaLiverHealth #VolunteerForHealth
We`re proud to announce the promotion of Kelly Black to Marketing Manager at Arizona Liver Health | Arizona Clinical Trials!
Kelly joined the AZ Liver Health team in early 2023, starting as a Marketing Coordinator and working her way up to Associate Marketing Manager by the summer of 2023. Her hard work and innovative ideas for the Commercial Operations team in the last year reflect her dedication to providing quality services to foster internal and external relationships and boost our organization’s brand recognition within our community and support the organization’s marketing and patient recruitment needs.
“I’m excited and honored to step into my new role as Marketing Manager. I’m incredibly grateful to Michelle Jones, my team, and our leadership for their support and encouragement here at ALH, ACT, and VEN,” says Kelly Black, Marketing Manager.
Help us congratulate Kelly on this well-deserved promotion and visit www.azliver.com for career opportunities!

A Big Milestone: Our First Phase 1 Patient!
We’re thrilled to share that we’ve welcomed our very first Phase 1 clinical trial patient at Arizona Liver Health! This is an exciting step toward finding new treatments and improving care for liver diseases, and we couldn’t be more grateful for the courage of our patients who make this research possible.
In this video, you’ll meet our first patient and hear about their journey through the trial process. Their story is a powerful reminder of how clinical trials are helping to shape the future of healthcare.
Watch the video to learn more and see how you, too, can be a part of something that could change lives!
Thank you to all who support this important work. Your participation could be the key to breakthroughs in liver disease care.
#LiverHealth #ClinicalTrials #PatientCare #Phase1Research #ArizonaLiverHealth #JoinTheJourney

We are excited to announce the promotion of Jane O`Neal, SHRM-CP to our new Director of Human Resources at Arizona Liver Health | Arizona Clinical Trials!
Jane has been part of the Arizona Liver Health family since April of 2019, starting as a Provider Liaison and working closely with both Dr. Anita Kohli and Dr. Naim Alkhouri, MD, FAASLD to learn about the organization, its operations, and its relationships within the community. In early 2021, Jane helped launch the company’s HR department and over the years, helped scale the company’s operations to its current workforce size while providing critical HR support regarding employee relations, talent recruitment, and benefits.
“I am thrilled to take on this new role/challenge and thank Dr. Kohli, Chaher Sakkal, and my HR team for their continued support for my career growth in HR, “ says Jane O’Neil, Director of HR.
Help us congratulate Jane on this well-deserved promotion and visit www.azliver.com for career opportunities!

Our CEO, Dr. Anita Kohli, was featured on the @tucsonblend to discuss how Arizona Clinical Trials is leading the charge in critical flu research!
We’re conducting studies on investigational medications to combat the flu virus—and you can be a part of it!
By participating in our clinical trials, not only will you help advance science and public health, but you may receive compensation up to $800 for trial related time and travel.
Join us and make a difference! Learn more and sign up today
👉 https://azclinicaltrials.com/flu-vaccine/
#ArizonaClinicalTrials #FluResearch #AdvanceScience #ClinicalTrials #TucsonMorningBlend #FightTheFlu #MedicalResearch #Tucson

We’re excited to share the news! Our brand new, 28,000 sq. ft. ACT Medical Park in Chandler, AZ is now open! This state-of-the-art center, brought to you by Arizona Liver Health (ALH) and Arizona Clinical Trials (ACT), offers access to groundbreaking clinical trials and advanced imaging —all aimed at improving healthcare solutions for you, this community and so many more lives around the world!
To our amazing patients, thank you! Your trust and support have helped us grow, and this new facility is a reflection of our commitment to you. It’s not just a building—it’s a promise to provide you with the highest quality care in an environment designed for your well-being. We look forward to continuing this journey together!
#PatientCare #ClinicalTrials #GrandOpening #YourHealthMatters

Today marks the 23rd anniversary of September 11, 2001 – a day that changed our nation forever. We honor the innocent lives lost and remember the incredible courage and sacrifice of the brave men and women who put others before themselves. Let this day remind us all that human kindness endures and remains unbreakable.

As we reflect on Labor Day, we are reminded of the incredible dedication of our healthcare professionals, who are truly the backbone of our community. Their tireless work ensures that each patient receives the highest quality care, and we are deeply thankful for all that they do.
This day also serves as a reminder of the significant advancements made possible by the labor movement, which has shaped the healthcare landscape, patient rights, and the working conditions that benefit us all.
Today, we not only celebrate the achievements of the labor movement but also express our profound gratitude to our medical staff for their unwavering commitment. Their contributions are essential to the progress we make together in advancing health and wellness.
#LaborDay #ALH #ACT #VEN #Dedication #Healthcare #HealthcareProfessionals #Celebrate #ThankYou
September is Primary Biliary Cholangitis (PBC) Awareness Month! 🌟
Primary Biliary Cholangitis (PBC) is a rare autoimmune liver disease that primarily affects women between the ages of 40 and 60, but it can impact others too. PBC often starts quietly, with symptoms like itching, fatigue, and brain fog. As the disease progresses, more severe symptoms like jaundice and abdominal pain may appear. Early detection and treatment are key to managing PBC and improving outcomes.
This September, let`s shine a light on Primary Biliary Cholangitis (PBC) and foster understanding. PBC is often misunderstood, it`s not related to alcohol use—it`s a serious condition that warrants our attention. By raising awareness, we can empower those living with PBC and support early diagnosis, leading to better outcomes and a stronger community.💙
#PBCAwareness #LiverHealth #SeptemberAwareness #EmpowerPBC
Exciting news! 🎉 We`re thrilled to announce the opening of our new, state-of-the-art medical center! At ACT Medical Park, we`re leading the way in healthcare innovation with a range of initiatives including:
ACT Phase 1 Clinical Trials Unit with 24 private rooms
-Participants may receive compensation for trial related time and travel up to $4000
-Experienced Care Team
-Join a trial and make a difference!
Arizona Clinical Trials Phase 2-4 clinic
-Participants may receive compensation for trial related time and travel
-Call today to find out about available trials you may be eligible for:
Vaccine Trials:
-COVID-19
-Influenza (flu)
-RSV
-Obesity/Weight Loss Trials
ACT Imaging (advanced research imaging capabilities including 3T MRI, MRI-PDFF, MRE, PET/ CT, X-ray, DEXA, OPTOS, and Ultrasound)
Arizona Liver Health standard of care clinic:
-Providing state-of-the-art, innovative and compassionate care to patients affected by liver diseases
-Over 30 years of combined experience, our team is equipped to provide liver disease patients with better outcomes and treatment options
-Call today to schedule a free screening of your liver!
-VEN Centers screening and treatment clinic
-ALH |VEN Pharmacy staff
Call today to join a clinical trial and help to revolutionize healthcare in your area!
#HealthcareInnovation #GrandOpening #ACTMedicalPark

Celebrate freedom, unity, and the American spirit this 4th of July! Let’s honor the bravery of those who fought for our independence and enjoy the fireworks with loved ones. Here`s to a day filled with pride, joy, and patriotism!

Hey everyone! Did you know that participating in Phase 1 studies can be a rewarding experience in more ways than one? Here are some fun facts that might surprise you:
Be a Trailblazer! - As a Phase 1 participant, you are among the first to test groundbreaking treatments and innovations. You`re truly a pioneer in the world of medicine!
Help Shape the Future! - Your participation plays a crucial role in the development of new therapies that can save lives and improve health outcomes for millions of people.
Get the Inside Scoop! - Gain a unique insight into the clinical research process and witness firsthand how new drugs are developed.
Earn While You Help! - Participants often receive compensation for their time and travel.
Comprehensive Health Checks! - Enjoy a thorough health check-up and monitoring throughout the study. It`s a great way to stay on top of your health.
Join a Community! - Connect with like-minded individuals who share your passion for advancing medical research. It`s a fantastic way to make new friends and build a supportive network.
Flexibility! - Many Phase 1 studies offer flexible scheduling to fit your lifestyle, making it easier for you to participate.
Ready to make a difference? Become a Phase 1 participant today and be a part of something extraordinary!
#AzClinicalTrials #MedicalResearch #Phase1 #ScienceForTheFuture #JoinUs

Interested in clinical trials but unsure where to start or what you qualify for? Click the link in our bio to be contacted about eligibility and stay updated on future trials!
#clinicaltrials #volunteer #participatetoday #azclinicaltrials

As Pride Month comes to a close, let`s carry the spirit of love, acceptance, and equality forward every day. This month has reminded us of the power of unity and the importance of standing together. Here`s to a future where everyone can be their true, authentic selves.
#PrideMonth

Join Our Phase 2/3 Clinical Trials!
Are you passionate about advancing medical research and contributing to groundbreaking health solutions? We are currently seeking healthy volunteers for our Phase 2/3 clinical trials!
-Why Participate?
*Make a Difference: Play a crucial role in the development of new treatments.
*Comprehensive Health Assessments: Receive thorough medical check-ups and monitoring.
*Potential Compensation Could be Provided: Eligible volunteers may be compensated for their time and participation.
-Who Can Join?
*Healthy Adults: Aged 18-65
*No Chronic Medical Conditions
*Willing to Comply with Study Requirements
-How to Apply:
*Visit our website azclinicaltrials.com
*Call us at 480-360-4000
Your participation can help pave the way for innovative therapies and improve lives worldwide. Join us in this vital journey towards better health!
#AzClinicalTrials #MedicalResearch #HealthyVolunteers #Health #MakeADifference #JoinUs

Today we honor Juneteenth, a day that marks the end of slavery in the United States and celebrates freedom, resilience, and the ongoing fight for justice. Let’s reflect on the struggles and triumphs of the past, and commit to building a future of equality and inclusion for all. #Juneteenth #ACT #ALH #VEN #CRIOH #FreedomDay #EqualityForAll

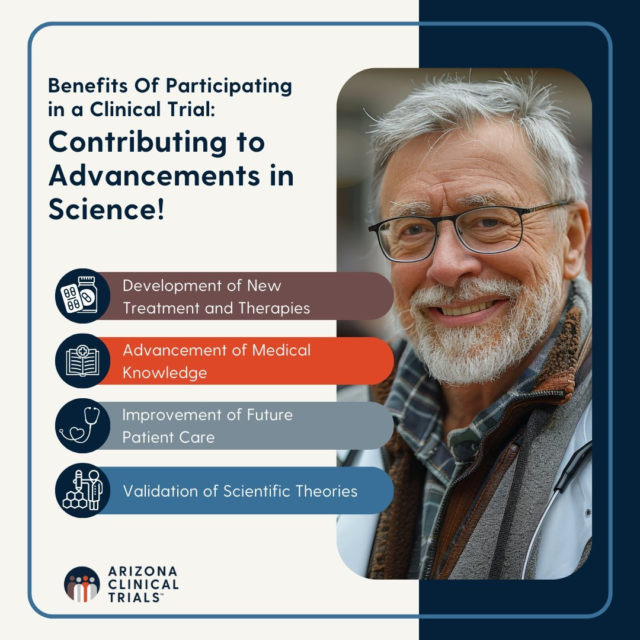
Participating in a clinical trial offers many benefits, especially in advancing science. Here are four key reasons:
1.Development of New Treatments:
Clinical trials help create and approve new treatments. Participants provide data on how well new drugs or devices work and how safe they are, which is crucial for making these treatments available to everyone.
2.Advancing Medical Knowledge:
Participants help researchers understand diseases better. The data collected shows how diseases work and how different people respond to treatments, leading to more effective future therapies.
3.Improving Future Patient Care:
The results from clinical trials improve medical guidelines and treatments. By volunteering, participants help ensure that future patients receive better, evidence-based care.
4.Validating Scientific Theories:
Clinical trials test scientific theories to confirm if they are correct. This rigorous testing ensures that only proven treatments are used in medical practice, driving scientific progress.
If you are ready to help advance scientific research by participating in a clinical trial, contact us today! www.azclinicaltrials.com
In clinical trials, particularly those involving new drugs or treatments, there are several phases. Each phase has a specific purpose and involves different types of participants. Phases 2 and 3 are critical stages in the development of a new treatment, and here`s a detailed explanation focusing on the early detection of adverse events in healthy volunteers:
Clinical Trial Phases Overview
Phase 1: Primarily focuses on safety. A small group of healthy volunteers (or patients) receive the treatment to determine its safety and dosage range and to identify side effects.
Phase 2: Involves a larger group of people (usually patients with the condition the drug aims to treat) to assess efficacy and further evaluate safety.
Phase 3: Expands to an even larger group of patients to confirm effectiveness, monitor side effects, compare it to commonly used treatments, and collect information that will allow the treatment to be used safely.
In some cases, Phase 2 and Phase 3 trials are combined. This approach can speed up the drug development process by allowing for more rapid progression from early efficacy assessments to large-scale confirmation of effectiveness and safety. In a Phase 2/3 clinical trial involving healthy volunteers, the primary focus is on the early detection of adverse events to ensure participant safety, optimize dosing, and provide essential safety data for regulatory approval. Through rigorous monitoring and data analysis, researchers aim to identify and manage any negative effects of the treatment promptly, contributing to the overall goal of developing safe and effective new therapies.

Join us in paying tribute to and remembering the U.S. military personnel who made the ultimate sacrifice while serving in the Armed Forces. We are forever grateful for their service.
Why Should You Volunteer in a Phase 1 Research Trial?
1. Helping Science and Medicine
When you volunteer for a Phase 1 research trial, you`re helping scientists and doctors figure out if new medicines are safe. Your participation is important because it helps companies and physicians understand how much of a new treatment is safe to give to patients. By being a volunteer, you`re playing a big role in helping create new medicines that can help a lot of people in the future.
2. Getting a Health Check-Up
Volunteers in these trials get detailed health check-ups. This means doctors will do physical exams, blood tests, and other health checks. These tests can help you learn a lot about your health and catch any issues early on. It`s like getting a really thorough check-up that can help you stay healthy.
3. Learning New Things
Being part of a Phase 1 trial is also a great learning experience. You`ll see how new medicines are tested and learn about the steps scientists take to make sure they are safe. You might also learn about the rules and ethics that guide medical research. This can be really interesting and give you a better understanding of how new treatments are developed.
4. Potential Financial Compensation
As a volunteer, you may receive compensation for your time spent participating in a trial.

Meet Angie Coste, our Phase 1 Clinical Research Director! Angie`s role is pivotal in our team as she oversees the planning, implementation, and management of Phase 1 clinical trials during drug development.
"Phase 1 research gives us the opportunity to be in the forefront of drug development and hepatic impairment studies gives us the opportunity to work with a sicker population who often benefit from our family-like team” - Angie Coste
These trials are the initial step in testing new treatments on human subjects, focusing on safety, dosage range, and potential side effects. Angie ensures that everything runs smoothly, from participant recruitment to safety monitoring and data management. Her expertise is essential in gathering crucial information that paves the way for later stages of clinical testing. #Phase1Research #TeamSpotlight

Why participate in clinical research?
1. Exclusive Availability
By joining a Phase 2 or Phase 3 clinical trial, you can be one of the first to receive promising new treatments or vaccines that are still being tested. These treatments aren’t available outside of the clinical trial setting, so you get a unique chance to try the latest innovations in medicine.
2. Potential for Better Outcomes
If you have a condition with limited treatment options or want to be part of new improved vaccines, new therapies or vaccines offered in these trials could lead to better health outcomes. The clinical trial treatments might provide relief or improvement giving you new hope and options.
3. Inclusion of Novel Therapies
These trials often include the latest advancements in medical technology, like gene therapies, targeted treatments, immunotherapies and advanced vaccine options. By participating, you gain access to cutting-edge medical innovations and the most recent discoveries in treatment.
4. Potential for Financial Compensation
As a participant, you may also receive financial compensation.
If you’re interested in participating in a clinical research trial, give our team a call to find out what clinical trials we currently are offering! We’d be happy to discuss your options and schedule an appointment for you.

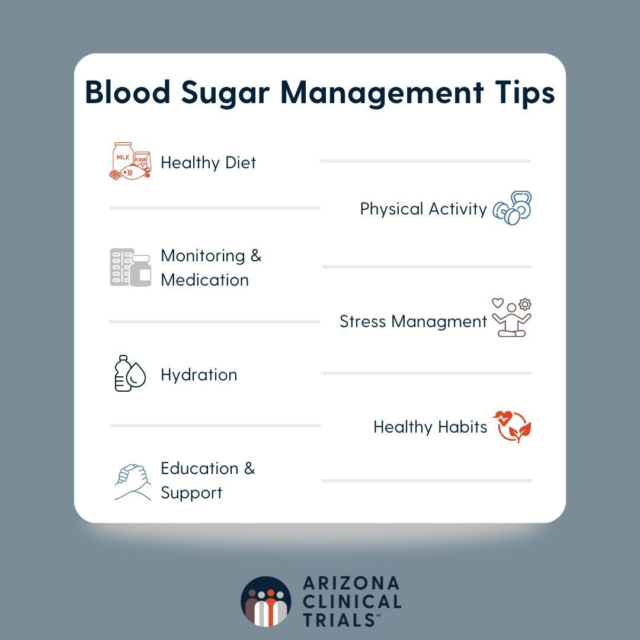
Quick Tips for Managing your Blood Sugar!
1. Healthy Diet
- Balance Carbohydrates
- Fiber-Rich Foods
- Portion Control
- Regular Meals
2. Physical Activity
- Regular Exercise
- Strength Training
- Consistency
3. Monitoring and Medication
- Regular Monitoring
- Medication Adherence
- Continuous Glucose Monitors
4. Stress Management
- Relaxation Techniques
- Sleep Hygiene
5. Hydration
- Stay Hydrated
6. Healthy Habits
- Avoid Smoking
- Limit Alcohol
7. Education and Support
- Continuous Learning
- Support Systems
Today, on Clinical Trials Day, we express our immense gratitude for the opportunity to contribute to enhancing patient care. Clinical trials are the backbone of healthcare innovation, driving forward new treatments and therapies that improve lives. We celebrate the dedication of researchers, healthcare professionals, and participants who make these advancements possible.

Common FAQs from a Phase 1 Healthy Volunteer!
Who Can Participate as a Healthy Volunteer? Qualifications and eligibility criteria, such as age, health status, and medical history are considered per study for individuals interested in volunteering for Phase 1 trials.
What is Expected of Participants? Participants must provide informed consent, attend study visits, undergo medical assessments, follow study protocol, take investigational medication, complete questionnaires, and potentially complete overnight stays in the clinic when participating in a trial.
What are the Benefits of Participation? Participating in a clinical trial as a healthy volunteer offers the opportunity to contribute to medical research, receive comprehensive health assessments, and potentially receive compensation for time and travel expenses.
Is Compensation Provided? Participants may receive compensation for time and travel.
How Can I Learn More? To learn more about participating in a clinical trial, contact us!

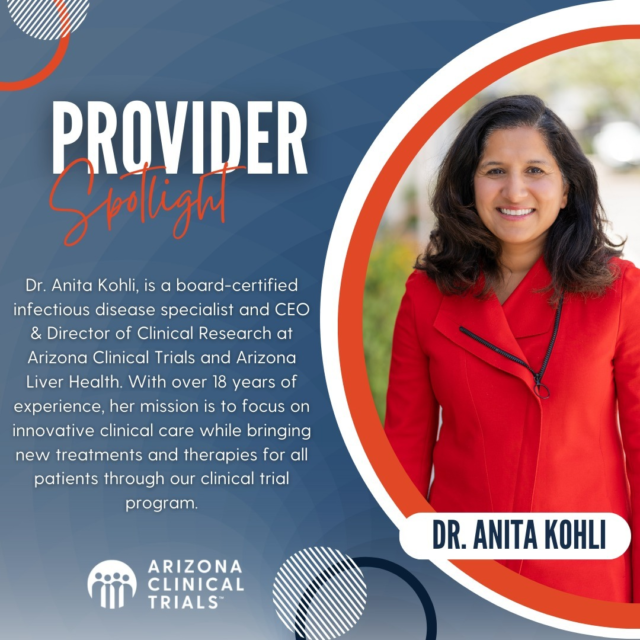
Meet Dr. Anita Kohli, MD: Infectious disease specialist, CEO, and Director of Clinical Research at Arizona Clinical Trials. With national and international acclaim, Dr. Kohli leads groundbreaking research on liver conditions and infectious diseases. Her expertise spans clinical and translational research, where she serves as lead investigator in numerous studies. A sought-after advisor, Dr. Kohli`s impact extends to viral hepatitis, COVID-19, drug development, and liver research advancement.
#InfectiousDisease #LiverHealth #ResearchLeader #act #azclinicaltrials #azliver

Healthy Eating Tips:
Prioritize Whole Foods: Choose whole, unprocessed foods as the foundation of your diet. Fruits, vegetables, whole grains, lean proteins, and healthy fats provide essential nutrients and fiber, supporting overall health and well-being.
Practice Portion Control: Pay attention to portion sizes to prevent overeating. Use smaller plates and utensils, and listen to your body`s hunger and fullness cues. Eating mindfully and slowly can help you recognize when you`re satisfied, rather than overly full.
Stay Hydrated: Drink plenty of water throughout the day to maintain hydration. Water supports various bodily functions, including digestion, metabolism, and temperature regulation. Limit sugary beverages and opt for water, herbal tea, or infused water as healthier alternatives.
#HealthyEatingTips #act #azclinicaltrials

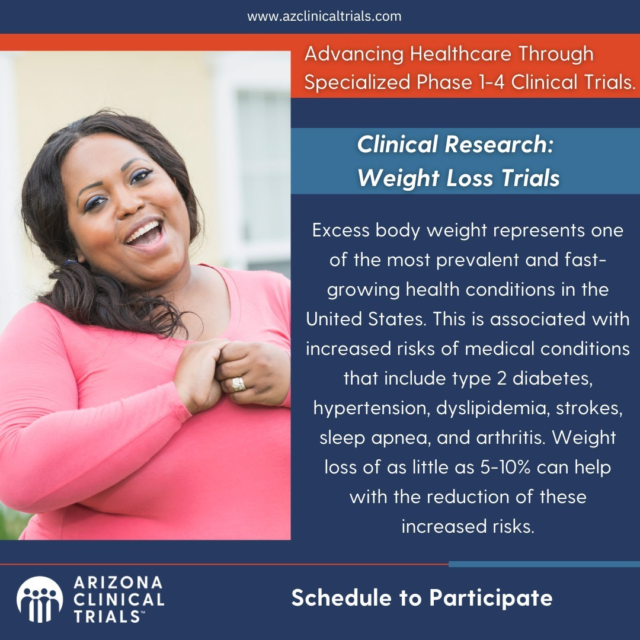
Discover cutting-edge healthcare advancements with our specialized Phase 1-4 Clinical Trials.
Learn more about Clinical Research focusing on Weight Loss Trials. With over 40% of the US population grappling with excess weight, it`s time to address this prevalent health concern. Excess weight correlates with heightened risks of type 2 diabetes, hypertension, dyslipidemia, strokes, sleep apnea, and arthritis. Even a modest weight loss of 5-10% can significantly mitigate these risks.
Join us in making a difference – schedule your participation today at www.azclinicaltrials.com.
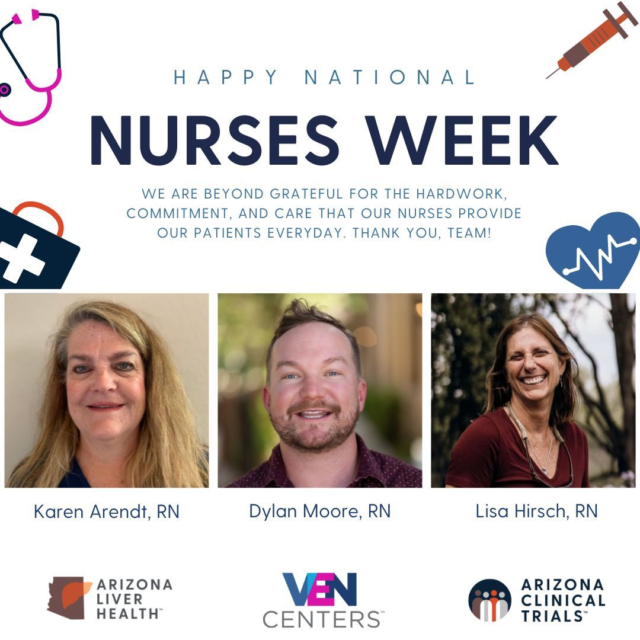
Happy National Nurses Week!
This week, we`re shining a spotlight on our exceptional Registered Nurses (RNs) as we celebrate National Nurses Week, running from May 6th to 10th. They`re the backbone of patient care nationwide, including at our ALH, ACT, and VEN Centers!
We deeply appreciate their unwavering dedication, hard work, and outstanding service, ensuring top-notch care for all patients.
A special shoutout to our onsite ALH nurses: a heartfelt thank you to Dylan Moore, Karen Arendt, and Lisa Hirsch for your invaluable contributions!
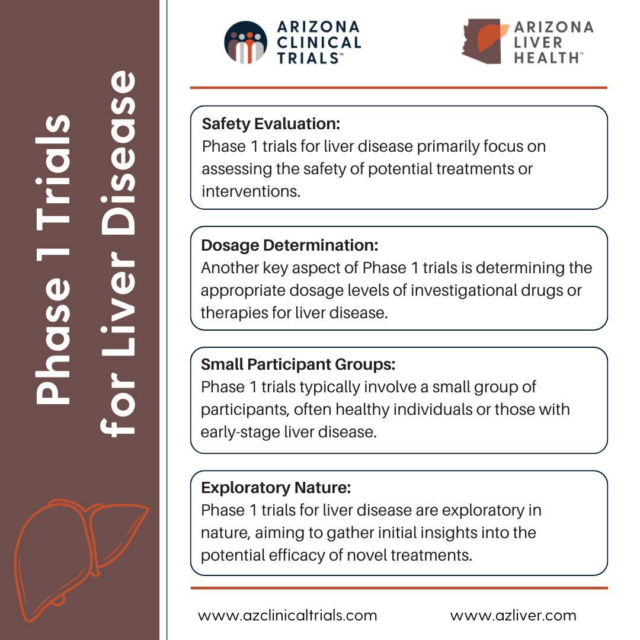
Discovering new hope for liver disease treatments! Phase 1 trials pave the way with safety evaluations, dosage determinations, and small participant groups. It`s a crucial first step towards breakthroughs in liver health.
Contact us today to see if a phase 1 liver trial might be right for you!
#phase1 #clinicaltrials #liverresearch
Exciting news! 🎉 We`re thrilled to announce the upcoming opening of our new, state-of-the-art medical center! At ACT Medical Park, we`re leading the way in healthcare innovation with a range of initiatives including:
ALH | VEN Pharmacy
Phase 1-4 Research Facilities
ACT Imaging
Arizona State Urological Institute
VEN Centers
Arizona Clinical Trials
Arizona Liver Health
As trusted partners for Pharmaceutical companies and Clinical Research Organizations (CRO), we pride ourselves on rapid trial start-up, efficient recruitment and enrollment, unwavering commitment to FDA regulatory compliance, and precise data collection.
Plus, with our cutting-edge facilities dedicated to clinical research, we`re equipped to provide evidence-based support for groundbreaking medical treatments and therapies. Stay tuned for more updates as we prepare to revolutionize healthcare in your area! #HealthcareInnovation #GrandOpening #ACTMedicalPark

Unlocking the Power of Diversity in Clinical Trials:
-Safety and Efficacy Across Populations: Different demographics respond uniquely to treatments. Diverse participation ensures safety and effectiveness for all.
-Ethical Imperative: Medical research should benefit everyone. Diverse trials address health disparities and ensure inclusivity in findings.
-Representation Matters: Tailoring treatments to diverse populations is crucial. Phase 1 trials with diverse participants enhance understanding and relevance.
-Combatting Bias: Excluding groups can skew results. Diversity in trials fosters comprehensive data, guiding informed decisions for safer, more effective treatments.
#ACT #ArizonaClinicalTrials #ClinicalTrials #DiversityInResearch

Phase 1 clinical trials represent the inaugural stage in testing novel drugs or therapies, involving a select group of volunteers. These trials meticulously assess safety, dosage, and potential side effects, laying the groundwork for transformative advancements in healthcare.
Learn more at www.azclinicaltrials.com
#ACT #ArizonaClinicalTrials #Phase1Research #Clinicaltrials
World Immunization Week celebrates the power of vaccines to protect people of all ages from preventable diseases. But behind every vaccine is rigorous clinical research. Clinical trials are vital for developing safe and effective vaccines. They help identify potential risks, determine dosage, and ensure efficacy.
Through research, we can enhance immunization programs, save lives, and create healthier communities.
If you are interested in supporting vaccine research and making a difference in the lives of our communities, contact us today! Arizona Clinical Trials is at the heart of vaccine research, seeking to improve patient outcomes, every step of the way.
#WorldImmunizationWeek #azclinicaltrials #act

We`re thrilled to announce the grand opening of our new Flagstaff, Arizona location. Did you know that 1 in 3 Americans suffer from Non-Alcoholic Fatty Liver Disease (NAFLD) or Non-Alcoholic Steatohepatitis (NASH) — and many are unaware of it?
At our Flagstaff location, we offer Fibroscan as an alternative to liver biopsy for detecting Fatty Liver Disease. Fibroscan is painless, non-invasive, requires no sedation, and can be completed in just minutes, enabling our providers to diagnose a patient`s condition during their visit.
Schedule your FREE Fibroscan appointment now!
(928) 863-1000
https://azliver.com/contact/locations/flagstaff-liver-clinic/

On this International World Health Day, let`s advocate for the universal right to health. Whether it`s accessing standard care for liver disease, participating in clinical research, or preventing hepatitis and STIs, everyone deserves quality healthcare. Let`s advocate for `My health, my right` worldwide.
#WorldHealthDay #MyHealthMyRight #azliver #azclinicaltrials #vencenters #crioh

Dive Deeper into Arizona Clinical Trials! At Arizona Clinical Trials, we`re committed to leading the way in medical research and innovation. Clinical trials stand as the cornerstone of medical advancement, offering a structured pathway to evaluate the safety and efficacy of new treatments, interventions, and medical devices. However, the success and impact of these trials are intricately tied to their focus.
Here`s why we stand out stand out:
👩⚕️ Experienced Providers: With years of expertise, our team ensures the highest standards of care and precision in every trial.
❤️ Compassionate Participant Care: Beyond just treatment, we offer a supportive environment where your needs and comfort come first.
🏥 Comfortable Facilities: Our state-of-the-art clinics are designed to make your experience as pleasant and stress-free as possible.
🚗 Transportation Assistance: Don`t let logistics hold you back. We provide convenient transportation options to ensure you never miss an appointment.
🔬 Specializing in Phase 1-4 Trials: From groundbreaking initial studies to large-scale evaluations, we cover the spectrum of clinical research to bring new treatments to life.
💪 Advancing Global Healthcare: Your participation isn`t just about personal benefit—it`s about shaping the future of healthcare for people everywhere.
Ready to be a part of something bigger? Join us at Arizona Clinical Trials and help pave the way for tomorrow`s medical breakthroughs! Contact us today to learn how you can get involved. #ClinicalResearch #MedicalInnovation #ArizonaClinicalTrials 🌐🌟
April is Defeat Diabetes Month! Let`s come together to raise awareness and take meaningful action against this prevalent health concern. Did you know that diabetes isn`t just about blood sugar levels? It`s also closely linked to liver disease. If you`re living with diabetes, it`s crucial to prioritize your liver health too. Consider getting a fibroscan, a non-invasive test that assesses liver health, especially if you`ve been diagnosed with diabetes.
Moreover, if you`re overweight and living with diabetes, there are exciting research opportunities available for you to participate in. By joining research studies, you can contribute to advancements in diabetes management and treatment options. Let`s empower ourselves with knowledge, prioritize our health, and work towards defeating diabetes together! 💪
#DefeatDiabetes #LiverHealth #ResearchOpportunities #TakeAction #ALH #ArizonaLiverHealth #ACT #ArizonaClinicalTrials

National Doctors` Day is a time to honor and appreciate the incredible dedication, skill, and compassion of medical professionals worldwide. Celebrated on March 30th in many countries, this day recognizes the invaluable contributions doctors make to our lives every day. From diagnosing illnesses to providing treatments and saving lives, doctors play a vital role in keeping us healthy and improving our well-being. Let`s take a moment to express our gratitude to these tireless heroes who work tirelessly to care for us. Thank you to our own Arizona Liver Health, Arizona Clinical Trials, CRIOH and VEN doctors, for your unwavering commitment and selfless service to humanity.
#NationalDoctorsDay 🩺👩⚕️👨⚕️#ALH #ArizonaLiverHealth #ACT #ArizonaClinicalTrials #VEN #ClinicalResearchInstituteofOhio
We are excited about the upcoming World Vaccine Congress! Can`t wait to join experts from around the globe to dive into the latest developments. Let`s connect and explore how Arizona Clinical Trials can elevate your clinical trial research programs.
We`re thrilled for the chance to network and forge potential partnerships. With our diverse participant pools, rapid trial kick-offs, and adaptive recruitment methods, along with cutting-edge facilities and excellent patient care, we`re primed to be your trusted collaborator.
Interested in setting up a meeting? Reach out to Michelle Jones directly via email at [email protected] or connect with her on LinkedIn to schedule a meeting. Looking forward to seeing you there!

Meet David!
David is our Study Start-up Specialist at Arizona Liver Health & Arizona Clinical Trials and an amazing contributor to the success of our organization. He believes in empowering patients to take control of their health and well-being, offering support for tangible lifestyle changes.
Here is what Clarissa, Director of Regulatory had to say about David,
"David expertly collaborates with sponsors, CROs, and the ALH team to ensure a prompt and efficient study start-up process by maintaining open communication channels."

Happy National Nutrition Month! We know the importance of healthy, nutritional choices and want to continue to encourage you to build nourishing habits.
Here`s a few tips to get you started:
-Reduce meal portion sizes
-Substitute carbohydrates with proteins and salads
-Integrate baked, boiled, and steamed foods over fried options
-Follow a diet rich in fruits and vegetables
-Avoid sugary beverages
If you have any questions, contact us! Our providers are a great resource for going over the nutrition plan that is best for you.
Click the link in our bio or visit www.azclinicaltrials.com
#nutritionmonth

Wishing everyone a joyful International Women`s Day! Supporting and empowering women enriches us all, each day and always.
On this special occasion, we take pride in our team, where 78% are remarkable women who contribute immensely to our success. Let`s continue to champion women in our communities, workplaces, and homes.
#InternationalWomensDay
@anita @ann mooore, tessa, @kelly dale, angie coste, @sachdeva, @kelly Black, @desirae anne p, @michelle j, @jane oneal, @any other women you can think of that may be on line with our company
Exciting news! Our newest Flagstaff office is officially open for business! Now, under one roof, you`ll find the dedicated teams of Arizona Liver Health, Arizona Clinical Trials, and VEN Centers.
We will continue to expand our capabilities at this location, but we are excited to offer Free Fibroscans, Hepatitis B and Hepatitis C testing and treatment, PrEP/PEP services in office, and NAFLD/NASH standard of care telemedicine visits.
We can`t wait to welcome you to our new space!
#ALH #ACT #VEN #Flagstaff

Are you ready to take charge of your health journey? We`re offering a unique opportunity for individuals aged 18 and older who are struggling with excess weight or are at risk of metabolic diseases. By joining our weight loss trials, you`ll not only embark on a path to a healthier you but also contribute to cutting-edge research in weight management. Your participation could pave the way for groundbreaking discoveries in the field.
Benefits:
✅ Personalized weight loss programs
✅ Expert guidance and support
✅ Help advance medicine
Don`t miss out on this chance to redefine your health and make a difference! Sign up today to start your journey towards wellness. Click the link in our bio to learn more #AzClinicalTrials #ClinicalTrials #HelpadvanceMedicine

It`s Phlebotomists Recognition Week!
Let`s celebrate the incredible contributions they make to healthcare. A huge shoutout to our phlebotomists in our clinics and research department—thank you for your dedication to our patients and advancing medical research!
#PhlebotomistsWeek #azliver #azclinicaltrials #crioh
Dr. Anita Kohli is a board-certified infectious disease specialist and CEO and Director of Clinical Research at Arizona Liver Health and Arizona Clinical Trials in the state of Arizona. Dr. Kohli has over 18 years of experience in the field of liver disease, treats viral hepatitis and NASH, and leads much of the country’s cutting-edge research in liver disease. She is a nationally and internationally recognized expert in clinical and translational research and has been the lead/principal investigator in multiple studies on various liver conditions as well as numerous publications in respected medical journals including JAMA, Lancet, and the Annals of Internal Medicine. Dr. Kohli sits on many advisory boards related to infectious disease such as viral hepatitis and COVID-19, drug development, and other liver and research development areas.
Dr. Kohli started Arizona Liver Health after serving as the Director of Research, Division of Hepatology and Chair of Research, Department of Internal Medicine, at St Joseph’s Hospital and Medical Center (now Common Spirit) in Phoenix, AZ. Prior to St. Joseph’s, Dr. Kohli was a clinical investigator at The National Institutes of Health, a physician at the National Heart, Lung, and Blood Institute, and completed fellowship in infectious diseases at the National Institutes of Health.
Dr. Kohli’s mission is to focus on innovative clinical care and the pursuit of excellence through scholarly activity and emphasizes academic involvement as part of the clinic culture serving several regions throughout the state. Dr. Kohli provides her patients with most cutting-edge options and exceptional patient experiences, and access to the best and latest state-of-the art treatments and studies.
#ArizonaClinicalTrials #ACT #ProviderSpotlight #DrKohli #ClinicalResearch
Today marks the beginning of Black History Month, a month-long event to celebrate the history, culture, and contributions of African Americans to our nation. Acknowledging the profound impact and indelible legacy of Black history, because understanding the past is key to building a more inclusive future.
#BlackHistoryMonth #ALH #ACT #VEN #CRIOH

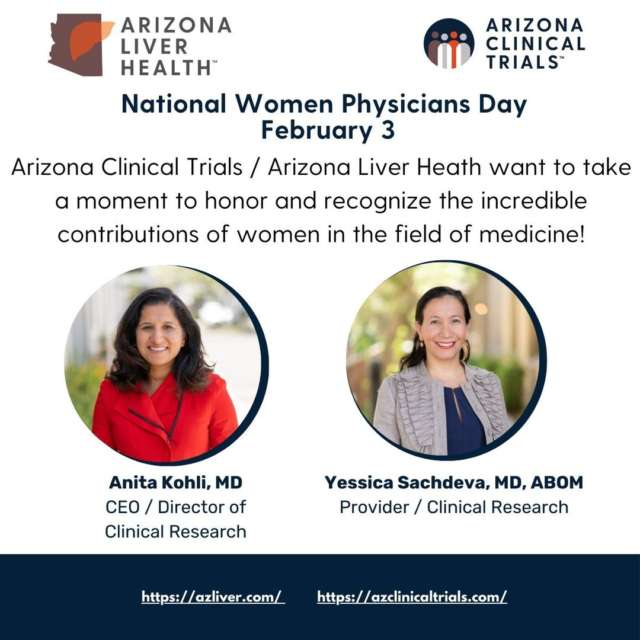
Today, on National Women Physician Day, we want to take a moment to honor and recognize the incredible contributions of women in the field of medicine and espicially our own Dr. Anita Kohli and Dr. Yessica Sachdeva who`s dedication, compassion, and expertise have not only improved patient care but have also paved the way for future generations of women in medicine.
From pioneers like Dr. Elizabeth Blackwell, the first woman to receive a medical degree in the United States, to the countless women physicians today who continue to push the boundaries of what`s possible, we owe them a debt of gratitude.
Today, let`s celebrate the achievements and contributions of women physicians worldwide. Thank you for your tireless dedication and for being role models for aspiring healthcare professionals. Your impact is immeasurable, and you inspire us every day.
#NationalWomenPhysicianDay #WomenInMedicine #HealthcareHeroes
Ever found yourself curious about the different phases of clinical trials? Check out what you need to know about phase 1 trials and what participating may look like for you!
Give us a call to sign up for a phase 1 clinical trial today!
#phase1 #clinicalresearch #azliver #azclinicaltrials
For this month`s spotlight, we`ll be featuring Dr. Yessica Sachdeva. Dr. Yessica Sachdeva is an internal medicine specialist with over 12 years of healthcare experience. Affiliated with various hospital networks in Arizona, Dr. Sachdeva is well-known in the community. Dr. Sachdeva’s interests and areas of focus include metabolic conditions, obesity management, liver disease, infectious disease, and geriatric care. Often, Dr. Sachdeva volunteers her time to provide education to Spanish speaking communities about the importance of liver health and screening. In addition to screening and treating patients, Dr. Sachdeva also aids in running the research program at Arizona Liver Health in Chandler, AZ and is the primary investigator for the COVID-19 clinical trials at Arizona Clinical Trials in Mesa, AZ.
#ArizonaClinicalTrials #ACT #ProviderSpotlight

Join us as we celebrate the life, work, and legacy of Dr. Martin Luther King! Let`s continue the journey towards a more inclusive future together.

Participating in a weight loss trial can offer unique benefits. While weight loss drugs exist, trials often explore new approaches or combinations that might be more effective or have fewer side effects. By joining a trial, you`re contributing to scientific progress, gaining access to potentially innovative treatments, and receiving personalized attention from experts monitoring your progress closely. It`s a chance to be part of cutting-edge research that could improve not just your own health but also that of others in the future.
Contact us today to see if you qualify for participation in a weight loss trial!
#weightloss #clinicalresearch #act

Finding participants for clinical trials is often the most challenging part of completing a study. This is mainly due to the stigmatization associated with misconceptions or false information surrounding clinical trials. These stigmas serve as a barrier not only for clinical trial participation but also for individuals to seek health care in the first place.
Here at Arizona Clinical Trials, the participants are the number one priority - our physicians get involved early on to speak to the risks and benefits of the clinical trial. We provide detailed information about the study so potential participants can privately assess whether the study may be relevant to them. We also try to understand each person’s motivation to participate and make time to answer participant questions and concerns whenever they come up.
There is no denying the immense value of clinical trial research on public health. While the advancements from research may not always be visible, they have undoubtedly impacted our society. Arizona Clinical Trials comprises experienced clinical research coordinators passionate about finding innovative therapies for all patients. Our mission is to bring new treatments and therapies for all patients through our vibrant clinical trials program.
#ACT #ArizonaClinicalTrials #ClinicalTrials #Research

Take charge of your health journey! Join our weight loss trial for people with excess weight and diabetes. Let`s work together towards healthier, happier lives! #WeightLossTrial #ACT

Warm wishes and joyous celebrations from Arizona Clinical Trials! May this holiday season be filled with laughter, love, and cherished moments. As we reflect on the year, we`re grateful for your continued support and participation. Here`s to a wonderful season and an amazing year ahead! Happy Holidays from all of us at ACT!
#happyholidays

Ok, so you have fatty liver disease....now what? Well, everyone`s liver journey is uniquely their own; treatment options will look different for everyone based on severity, stage, and other specific variations that contribute to the progression of the disease. At Arizona Liver Health, prioritizing your health is our number one priority. We offer the latest advancements in technology that can improve your health with an easy step-by-step program designed specifically for you! Learn more about your condition and how Arizona Liver Health can help.

There`s immense value in clinical research. With new and emerging diseases constantly threatening global health, it’s more important than ever to participate in clinical research trials. In addition to saving millions of lives per year, clinical research advancements have the power to prevent diseases from spreading and protect vulnerable individuals from potentially deadly infections. Are you ready to make a difference? Click the link in our bio to learn more about how you can participate. Making a change tomorrow starts with today!

